|
Case Report
Lone atrial fibrillation: A case report on a rare complication of pregnancy
1 Department of Medicine, The Brooklyn Hospital Center, 121 Dekalb Avenue, Brooklyn, NY 11201, USA
2 Division of Cardiology, The Brooklyn Hospital Center, 121 Dekalb Avenue, Brooklyn, NY 11201, USA
Address correspondence to:
Samridhi Sinha
Department of Medicine, The Brooklyn Hospital Center, 121 Dekalb Avenue, Brooklyn, NY 11201,
USA
Message to Corresponding Author
Article ID: 100014C03SS2023
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Sinha S, Devarakonda PK, Rodriguez CA. Lone atrial fibrillation: A case report on a rare complication of pregnancy. Edorium J Cardiol 2023;8(2):1–4.ABSTRACT
Atrial fibrillation (AF) is one of the most common arrhythmias and is a rare phenomenon seen in pregnant patients unless there is an underlying cardiopulmonary abnormality. Lone AF in pregnancy is a diagnosis of exclusion. A thorough workup including history, physical examination, imaging, and laboratory workup should be done diligently to exclude cardiopulmonary diseases (like hypertensive heart disease, congenital heart disease, valvular heart disease, asthma or chronic obstructive pulmonary disease, pulmonary embolism, rheumatic heart disease) and non-cardiac diseases (such as hyperthyroidism or electrolyte abnormalities or medications). There are very few case reports and studies published so far on this topic. This case report is on a pregnant patient without any significant past medical history who developed new-onset lone AF without any known cause and was managed with Diltiazem, which resulted in chemical cardioversion of atrial fibrillation with rapid ventricular rate to normal sinus rhythm.
Keywords: Anticoagulant, Antiarrhythmics, Cardioversion, Lone atrial fibrillation in pregnancy
INTRODUCTION
Atrial fibrillation (AF) in pregnancy is an uncommon phenomenon and the diagnosis is made by excluding any secondary causes like valvular heart disease, structural heart disease, asthma, obstructive sleep apnea, or other cardiopulmonary disease. Pregnant patients presenting as an AF should have an extensive workup including detailed history taking, physical examination, 12-lead electrocardiogram, complete blood count, basic metabolic panel with serum electrolytes, a thyroid function test, urine drug screen, and a transthoracic echocardiogram. Treatment of AF in pregnancy is challenging due to concern for teratogenicity associated with use of medications and side effects of anticoagulation. Direct current cardioversion is the treatment of choice in hemodynamically unstable patients, whereas controlling the heart rate is the primary treatment goal in patients who are hemodynamically stable.
CASE REPORT
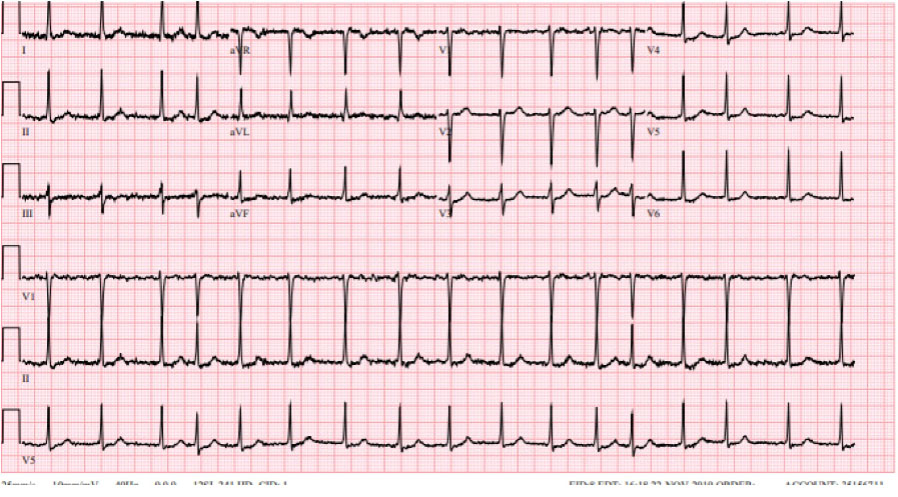
A 40-year-old female with no significant past medical history, P1021 at 29th weeks and 6 days of gestation, presented to the emergency department with a chief complaint of palpitations for 30–45 minutes along with sudden onset of diaphoresis, shortness of breath, and chest pain. In the emergency department, the patient was found to be in an irregularly irregular rhythm, and electrocardiogram showed atrial fibrillation with a ventricular rate of 101 beats per minute (Figure 1), blood pressure was 112/76 mmHg, respiratory rate 14/minute, and oxygen saturation of 98% on room air. The patient’s serum electrolytes, hemoglobin, hematocrit, and thyroid stimulating hormone were within the normal range, and the urine drug screen was negative. The imaging modality of choice for evaluation of pulmonary embolism in pregnant patients, which is the ventilation-perfusion scanning of lungs, ruled out pulmonary embolism. Transthoracic echocardiogram showed an ejection fraction of 60–65%, without any structural or valvular abnormalities.
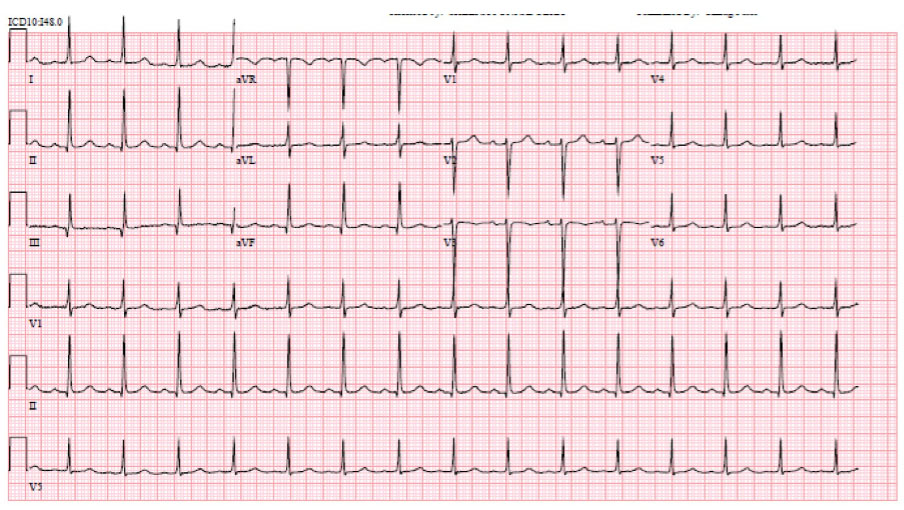
Initially, three intravenous pushes of Diltiazem were given without any resolution with heart rate going as high as 180 beats per minute with the rapid ventricular rate on the cardiac monitor and was subsequently started on Diltiazem drip at a rate of 10 mg/h. After which the patient’s echocardiogram showed cardioversion to normal sinus rhythm within 24 hours of beginning the Diltiazem drip (Figure 2). No probable cause of AF was found, so the patient was discharged home without any anticoagulation or antiarrhythmics, as risks overweigh the benefits of treatment with anti-coagulants and antiarrhythmics for lone AF.
DISCUSSION
Lone AF was coined 60 years ago in 1954 by Evans and Swann for patients in whom subsequent investigation shows that heart disease is absent [1].
During pregnancy, arrhythmias are triggered due to several physiological changes like an increase in cardiac output, heart rate, plasma volume, wall tension along with fluctuating hormonal levels, and reduction in systemic vascular resistance or sometimes due to the use of tocolytics [2]. Risk factors like increased maternal age, white race, male sex, obstructive sleep apnea, obesity, consuming alcohol, endurance sports, family history, and several recognized mutations could trigger the development of lone AF [2],[3].
The mechanism behind lone AF is still unclear. However, atrial ectopy, atrial enlargement, fibrosis, increased vagal tone are known to play a role. Genomic variations, microRNAs, and some changes in relevant biomarker levels have also correlated with lone AF [4].
Lone AF is a diagnosis of exclusion and is only confirmed after all the causes of AF are ruled out. Initial emergent workup should include a 12-lead electrocardiogram, complete blood count, basic metabolic panel with serum electrolytes, a thyroid function test, urine drug screen, and a transthoracic echocardiogram, an important implications for both maternal and fetal outcomes in management of lone idiopathic AF during pregnancy. First trimester is the period in which organogenesis takes place, developing fetus is highly sensitive to the potential teratogenic effects of medications. Drugs may have possible effects on fetal growth or lead to fetal arrhythmias in the second and third trimesters [5].
Many commonly used medications in AF like some beta-blockers and anticoagulants such as warfarin have been shown to increase the risks of adverse fetal outcomes [6],[7],[8],[9]. In hemodynamically unstable patients, direct current cardioversion is the treatment of choice; however, in hemodynamically stable patients controlling the heart rate is the primary treatment goal. Beta-blockers, non-dihydropyridine calcium channel blockers can be used as the first choice in pregnant patients. Digoxin can be used, but due to varying serum levels and its toxicity, especially during pregnancy, its use has been limited. Quinidine is one of the safest drugs used in pregnancy and can be used for pharmacological cardioversion as well. Antiarrhythmic drugs like sotalol, flecainide, or propafenone are also reported to be safe in a few studies [10].
CONCLUSION
Pregnancy is a hyperdynamic state and is associated with vasodilation of the systemic vascular resistance, increase in cardiac output, decrease in arterial pressures including systolic blood pressure, diastolic blood pressure and mean arterial pressure, and increase in heart rate. All these changes may predispose a pregnant patient to arrhythmias. As lone AF is a diagnosis of exclusion in pregnant patients, a careful history, examination, and a thorough workup for a secondary cause of arrhythmias should be ruled out before making a definitive diagnosis of lone AF of pregnancy. It is extremely challengi to treat lone AF of pregnancy because of concern for teratogenicity associated with medications and the use of anticoagulation during pregnancy.
REFERENCES
1.
Evans W, Swann P. Lone auricular fibrillation. Br Heart J 1954;16(2):189–94. [CrossRef]
[Pubmed]

2.
Lee MS, Chen W, Zhang Z, et al. Atrial fibrillation and atrial flutter in pregnant women—A population-based study. J Am Heart Assoc 2016;5(4):e00318. [CrossRef]
[Pubmed]

3.
Tello-Montoliu A, Hernández-Romero D, Sanchez-Martínez M, Valdes M, Marín F. Lone atrial fibrillation – A diagnosis of exclusion. Curr Pharm Des 2015;21(5):544–50. [CrossRef]
[Pubmed]

4.
Lin KB, Marine JE, Calkins H, et al. Should we abandon the term-lone atrial fibrillation? Hellenic J Cardiol 2019;60(4):216–23. [CrossRef]
[Pubmed]

5.
European Society of Gynecology (ESG); Association for European Paediatric Cardiology (AEPC); German Society for Gender Medicine (DGesGM); Regitz-Zagrosek V, Blomstrom Lundqvist C, et al. ESC guidelines on the management of cardiovascular diseases during pregnancy: The task force on the management of cardiovascular diseases during pregnancy of the European Society of Cardiology (ESC). Eur Heart J 2011;32(24):3147–97. [CrossRef]
[Pubmed]

6.
Vitale N, De Feo M, De Santo LS, Pollice A, Tedesco N, Cotrufo M. Dose-dependent fetal complications of warfarin in pregnant women with mechanical heart valves. J Am Coll Cardiol 1999;33(6):1637–41. [CrossRef]
[Pubmed]

7.
Sadler L, McCowan L, White H, Stewart A, Bracken M, North R. Pregnancy outcomes and cardiac complications in women with mechanical, bioprosthetic and homograft valves. BJOG 2000;107(2):245–53. [CrossRef]
[Pubmed]

8.
Lydakis C, Lip GY, Beevers M, Beevers DG. Atenolol and fetal growth in pregnancies complicated by hypertension. Am J Hypertens 1999; 12(6):541–7. [CrossRef]
[Pubmed]

9.
Yakoob MY, Bateman BT, Ho E, et al. The risk of congenital malformations associated with exposure to β-blockers early in pregnancy: A meta-analysis. Hypertension 2013;62(2):375–81. [CrossRef]
[Pubmed]

10.
Kozlowski D, Budrejko S, Lip GYH, et al. Lone atrial fibrillation: What do we know? Heart 2010;96(7):498–503. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Samridhi Sinha - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Pradeep Kumar Devarakonda - Acquisition of data, Analysis of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Cesar Ayala Rodriguez - Conception of the work, Design of the work, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2023 Samridhi Sinha et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.