|
Research Article
A single-center study: Predictive accuracy of Positron Emission Tomography (PET) stress testing for ischemic cardiac complications in liver transplant patients
1 Department of Hospital Medicine, Cypress Fair Banks Medical Center, Houston, Texas, USA
2 Imo State University, Owerri, Nigeria
3 Emory University, Atlanta, Georgia, USA
Address correspondence to:
Okechukwu Mgbemena
Department of Hospital Medicine, Cypress Fair Banks Medical Center, 10655 Steepletop Dr, Houston, Texas 77065,
USA
Message to Corresponding Author
Article ID: 100011C03OM2019
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Mgbemena O, Njoku C, Sears I, Okoroafor C, Wedd J. A single-center study: Predictive accuracy of Positron Emission Tomography (PET) stress testing for ischemic cardiac complications in liver transplant patients. Edorium J Cardiol 2019;5:100011C03OM2019.ABSTRACT
Aims: Posttransplant cardiac complications are well-known adverse events constituting a major cause of morbidity and mortality in patients undergoing liver transplantation regardless of etiology of chronic liver disease. To determine the predictive accuracy of Positron Emission Tomography (PET) stress testing for postoperative ischemic cardiac events in patients undergoing liver transplantation.
Methods: We evaluated 60-day postoperative cardiac complications for patients who had undergone PET stress testing for preoperative evaluation. Patients with end-stage liver disease (ESLD) who underwent liver transplantation between 2009 and 2015 were reviewed. Patient demographics, risk factors, and short-term postoperative cardiac complications were collected and statistical analysis was performed.
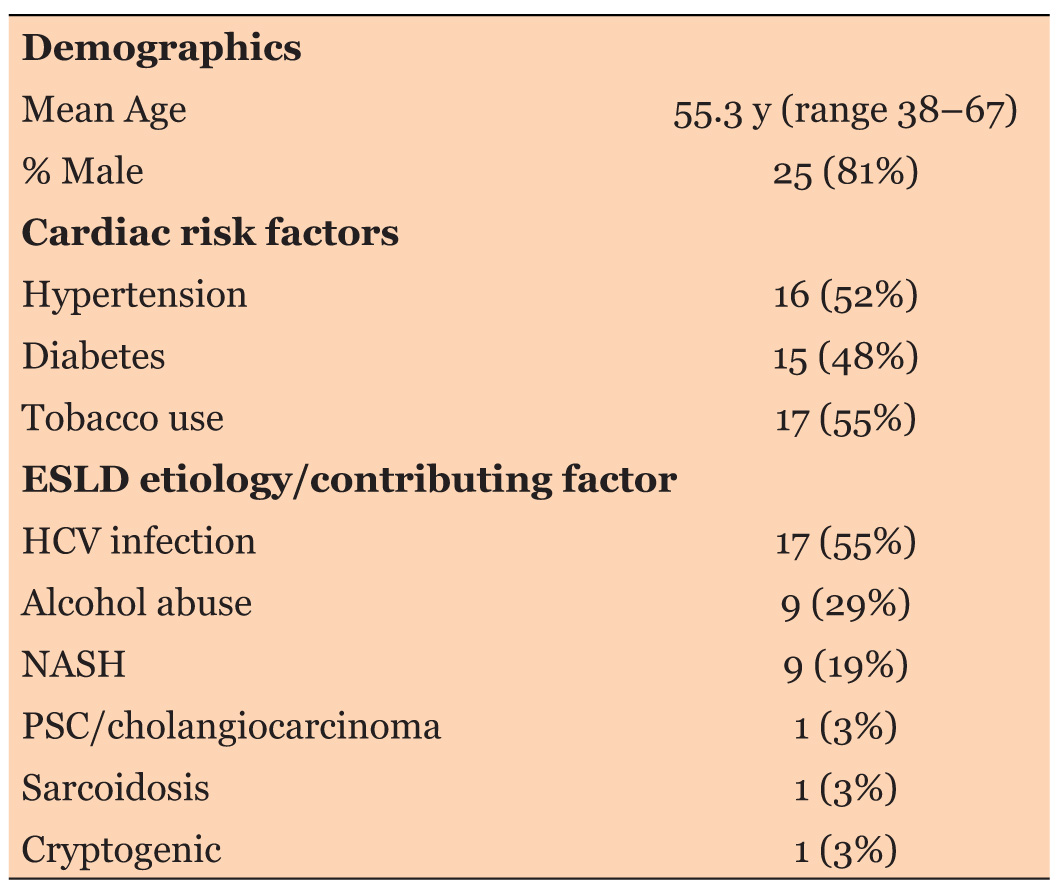
Results: A total of 31 patients (25 [81%] men and 6 (19%) women) with a mean age at transplantation of 55.3 year (range 38–67) were identified. Cardiac risk factors included diabetes 15 (48%), hypertension 16 (52%), and current/ former tobacco use 17 (55%). Contributing factors to ESLD were chronic HCV infection 17 (55%), alcohol abuse 9 (29%), NASH 9 (29%); PSC/ cholangiocarcinoma 1 (3%), sarcoidosis 1 (3%), and cryptogenic 1 (3%). Calculated MELD score for patients with preoperative labs ranged from 10.1 to 29.2. All 31 patients had a PET stress testing for preoperative assessment. 29 (93%) had a negative stress test. Post liver transplantation, only 1 (3%) patient had third degree atrioventricular (AV) blocks attributable to ischemia at 60-day followup. Other notable postoperative complications include hypotension 5 (16%), acute renal failure 5 (16%), acute pulmonary edema 2 (6%) and congestive heart failure 4 (13%).
Conclusion: PET stress testing has a high negative predictive value for postoperative acute coronary syndromes in liver transplant patients (Negative Predictive Value (NPV) = 96.5%, 95% confidence interval (CI) 96.22–96.88%).
Keywords: Cardiac pre-operative risk evaluation, Positron emission tomography, Stress testing
INTRODUCTION
Ischemic cardiac and neurologic complications remain a major concern for patients undergoing surgery with general anesthesia [1]. Few of ischemic complications include cerebrovascular accidents, myocardial infarction, heart blocks, and postoperative atrial fibrillation [2]. Risk factors that predispose to increased postoperative ischemic complications include: prior history of ischemic heart disease, prior history of stroke or vasculopathy, high-risk surgery – including vascular and intraperitoneal surgery; history of congestive heart failure, insulindependent diabetes, and presence of chronic kidney disease (Creatinine > 2) [3]. Some guidelines and/or risk stratification calculators are available for preoperative screening for cardiovascular events including the Revised Cardiac Risk Index (RCRI) for preoperative risk assessment [4]. Other similar risk calculators include American College of Surgeons National Surgical Quality Improvement Program (NSQIP) risk prediction calculators and Bilimoria ACS surgical risk calculator.
In general, patient at low cardiovascular risk and/or undergoing low-risk, non-cardiac surgery may not need further preoperative screening or evaluation. Patients at high risk of complications, unknown or poor functional capacity <4 METs) and/or undergoing high-risk surgery usually proceed to preoperative screening for Coronary Artery Disease (CAD) and subsequent revascularization and/or medical optimization prior to surgery if indicated [3],[5]. There are several modalities available to screening for CAD including exercise stress testing, Dobutamine stress testing, PET stress testing, Echo-stress testing, Nuclear Medicine stress testing, and Left Heart catheterization (LHC).
Of all the various modalities for CAD screening, exercise stress testing remains the preferred, firstline modality for CAD screening due to low cost and provision of additional information including patient’s exercise capacity [6]. Although exercise stress testing is firstline, patients may have contraindication to exercise stress testing e.g., presence of Left Bundle Branch Block (LBBB); baseline ST segment depression/elevation; recent myocardial infarction; severe aortic stenosis; uncontrolled arrhythmia and other baseline electrocardiogram (EKG) abnormalities that may interfere with accurate interpretation of stress EKG [7]. Other factors that limit use of exercise stress testing include patient’s inability to exercise on treadmill or chronotropic incompetence or heart block that may prevent patient from reaching acceptable heart rate – 85% of age-adjusted maximum heart rate [8].
When patients are unable to undergo exercise stress testing due to any of the above contraindications, other modalities including dobutamine stress testing, PET stress testing, echo-stress testing, nuclear medicine stress testing, or LHC can be used for CAD screening. Of all the available modalities, LHC is the most invasive but has benefit of al concomitant PerCutaneous Intervention (PCI) with balloon angioplasty, Bare Metal Stenting (BMS), or Drug-Eluting stenting (DES). Beyond the firstline, the exercise stress testing, the modality of choice varies across practices depending of availability at institution, expertise, cost, risk of contrast nephropathy or allergy, and patient preference.
The predictive accuracy of a screening modality refers to how accurate a screening tool is in determining if indeed there will be any ischemic postoperative complications. Two of the few ways to determine the predictive accuracy of a test include a Positive Predictive Value (PPV) and a Negative Predictive Value (NPV). A PPV is the probability that patients with a positive screening test truly have the disease while a NPV is the probability that patients with a negative screening test truly do not have the disease.
We evaluate, in this single-center study, the predictive accuracy of PET stress testing for ischemic cardiac complications in patients undergoing allogeneic liver transplantation due to end-stage liver disease (ESLD). Patients who had a negative PET stress testing for preoperative screening were monitored for up to 90 days postoperatively for any ischemic complications.
MATERIALS AND METHODS
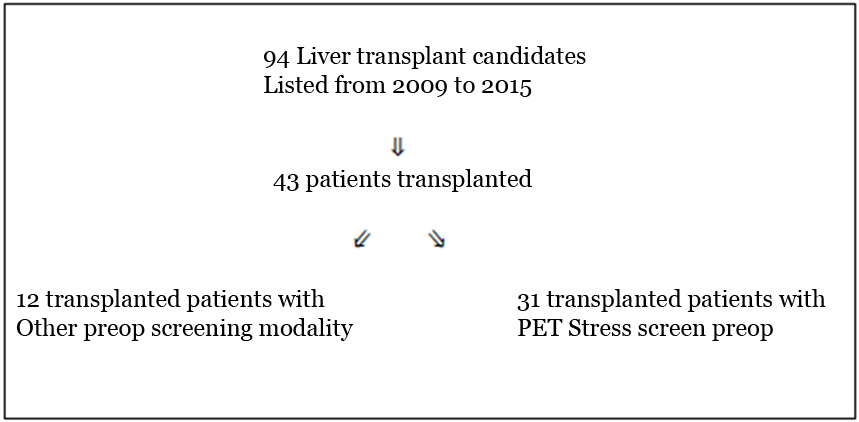
A list of 94 patients who had allogeneic liver transplantation in a major tertiary center from 2009 to 2015 was reviewed to evaluate the predictive accuracy of PET stress testing for postoperative ischemic complications. Patients had varying preoperative cardiac screening including left heart catheterization, non-invasive treadmill stress test, nuclear medicine stress testing, PET stress testing, and dobutamine stress testing. To evaluate postoperative accuracy of PET stress testing, patients who had PET stress for their preoperative evaluation were selected from the entire pool of patients. A comprehensive chart review was done and pertinent data, e.g., preoperative cardiovascular risk factors and lab values were documented. Patients were also followed postoperatively and any adverse events attributable to cardiac ischemia were documented. Ischemic events monitored postoperatively include ST-elevation Myocardial Infarction (STEMI); Non-STelevation myocardial infarction (NSTEMI); new bundle branch block or similar ischemic complications. As shown in Figure 1, a total of 94 patients were evaluated for liver transplantation within the timeframe noted above. Out of 94 patients evaluated, only 43 patients went on to have liver transplantation during that time interval. Out of the 43 liver transplant patients, 31 patients had PET stress testing as their modality of choice for preoperative cardiac screening. Medical records of those 31 patients were reviewed and documented evidence of postoperative ischemic events including STEMI, NSTEMI, or heart block were recorded. Chart review was done at 30-day, 60-day, and 90-day postoperatively. In addition, patient demographics including age at evaluation, sex, cardiac risk factors such as tobacco use, hypertension, diabetes, etiology of end stage liver disease, preoperative lab values including creatinine, total bilirubin, INR, and other pertinent data were recorded. These data are then used to determine predictive accuracy of PET stress testing for postoperative cardiac complications in this patient population. Data obtained were analyzed statistically.
RESULTS
In this tertiary institution, 94 patients with endstage liver disease (ESLD) were evaluated for liver transplantation between 2009 and 2015. 51 patients did not have liver transplantation for various reasons including but not limited to poor social support, lack of availability of matched donor liver, lack of insurance, and medication non-adherence. 43 patients had liver transplantation. Out of 43 patients who had a liver transplant, 31 patients had a PET stress test preoperatively for cardiac ischemic evaluation as shown in Figure 1.
Preoperative and postoperative data for all 31 transplanted patients who had PET stress testing were analyzed. Table 1 shows baseline characteristics. A total of 31 patients: 25 (81%) men and 6 (19%) women with a mean age at transplantation of 55.3 y (range 38–67) were identified. Cardiac risk factors include diabetes 15 (48%), hypertension 16 (52%), and current/former tobacco use 17 (55%). Contributing factors to ESLD are chronic HCV infection 17 (55%), alcohol abuse 9 (29%), Non-alcoholic Steato-Hepatitis (NASH) 9 (29%); Primary Sclerosing Cholangitis (PSC)/Cholangiocarcinoma 1 (3%), sarcoidosis 1 (3%), and cryptogenic 1 (3%). Calculated MELD score for patients with preoperative labs ranged from 10.1 to 29.2.
All 31 patients had a PET stress testing for preoperative assessment. 29 (93%) had a negative stress test. Post liver transplantation, only 1 (3%) patient had third degree AV blocks attributable to ischemia at 60-day follow-up. Other notable postoperative complications include hypotension 5 (16%), acute renal failure 5 (16%), acute pulmonary edema 2 (6%), and congestive heart failure 4 (13%).
Using the data above, the NPV of PET stress testing was calculated. PET stress testing has a high NPV for postoperative acute coronary syndromes in this patient cohort, NPV of 96.5% (95% CI 96.22–96.88%).
DISCUSSION
Perioperative ischemic cardiovascular and cerebrovascular accidents remain major contributor to morbidity and mortality following both cardiac and noncardiac surgery. Patient at low cardiovascular risk and/ or undergoing low-risk, non-cardiac surgery may not need further preoperative screening. Patients at high-risk of complications, unknown or poor functional capacity (<4 METs) and/or undergoing high-risk surgery usually proceed to preoperative screening for CAD and subsequent revascularization and/or medical optimization prior to surgery if indicated. For patients needing preoperative ischemic screening, there are several exercise, imaging, and invasive modalities available for CAD screening. These modalities include but not limited to Dobutamine stress testing, PET stress testing, echo-stress testing, Nuclear Medicine stress testing, and LHC. The test of choice often depends on availability at institution, expertise, cost, risk of contrast nephropathy or allergy, and patient preference.
We evaluate the predictive accuracy of PET stress testing in liver transplant patients at a major tertiary institution. We focus on monitoring patients for any cardiac postoperative complications that is attributable to ischemia in a cohort who had a negative PET stress testing preoperatively. Our endpoints include occurence of STEMI, NSTEMI, infrahisian bundle block attributable to ischemia; and other manifestation of perioperative cardiac ischemia.
Of the 31 patients who had preoperative PET stress testing, 29 (93%) had a negative stress test while 2 (7%) had a positive test and went on to have pre-operative LHC. All 31 patients went on to have allogeneic liver transplantation. Post liver transplantation, only 1 (3%) out of 29 patients with preoperative negative PET stress test had ischemic complications within 90 days after surgery. The patient had third degree AV blocks attributable to ischemia at 60-day follow-up. Other notable, non-ischemic postoperative complications include hypotension 5 (16%), acute renal failure 5 (16%), acute pulmonary edema 2 (6%), and congestive heart failure 4 (13%). Within this cohort, we found that PET stress testing has a high negative predictive value for postoperative acute coronary syndromes in liver transplant patients (NPV = 96.5%, 95% CI 96.22–96.88%), so therefore is an acceptable screening modality when there is a contraindication to or patient is unable to tolerate exercise stress testing. In review of literature [3],[4],[5], we found that non-invasive stress testing has a high negative predictive value and are very sensitive for screening of coronary artery disease in preoperative patients but we did not find literature specifically evaluating the negative predictive value, sensitivity and/or specificity of PET stress testing in preoperative patients. It is very noteworthy that our analysis is focused on limited patient population and is also limited by relatively small number of patients.
CONCLUSION
For patients at high-risk of complications, unknown or poor functional capacity (<4 METs) and/or undergoing high-risk surgery, exercise stress testing remains firstline for screening but when patients are unable to undergo exercise stress testing or have contraindications to exercise stress testing, PET stress testing is an acceptable alternative. PET stress testing has a high negative predictive value for postoperative acute coronary syndromes in liver transplant patients (NPV = 96.5%, 95% CI 96.22–96.88%).
REFERENCES
1.
Smilowitz NR, Gupta N, Ramakrishna H, Guo Y, Berger JS, Bangalore S. Perioperative major adverse cardiovascular and cerebrovascular events associated with noncardiac surgery. JAMA Cardiol 2017;2(2):181–7. [CrossRef]
[Pubmed]

2.
Smilowitz NR, Guo Y, Rao S, Gelb B, Berger JS, Bangalore S. Perioperative cardiovascular outcomes of non-cardiac solid organ transplant surgery. Eur Heart J Qual Care Clin Outcomes 2018;5(1):72–8. [CrossRef]
[Pubmed]

3.
Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery). Circulation 2007;116(17):e418–99. [CrossRef]
[Pubmed]

4.
Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100(10):1043–9.
[Pubmed]

5.
Mangano DT, Goldman L. Preoperative assessment of patients with known or suspected coronary disease. N Engl J Med 1995;333(26):1750–6. [CrossRef]
[Pubmed]

6.
Miller TD, Askew JW, Anavekar NS. Noninvasive stress testing for coronary artery disease. Cardiol Clin 2014;32(3):387–404. [CrossRef]
[Pubmed]

7.
Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: Summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). J Am Coll Cardiol 2002;40(8):1531–40.
[Pubmed]

8.
Hill J, Timmis A. Exercise tolerance testing. BMJ 2002;324(7345):1084–7. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Okechukwu Mgbemena - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Cornelius Njoku - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Isaac Sears - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Chidi Okoroafor - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Joel Wedd - Conception of the work, Design of the work, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2019 Okechukwu Mgbemena et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.