|
Case Report
A case of transient right ventricular failure secondary to severe pulmonary hypertension in setting of methamphetamine use
1 Internal Medicine, Southeast Health Medical Center, Dothan, Alabama, USA
2 Internal Medicine, Alabama College of Osteopathic Medicine, Dothan, Alabama, USA
Address correspondence to:
Paramjit Kaur
Internal Medicine, Southeast Health Medical Center, Dothan, Alabama,
USA
Message to Corresponding Author
Article ID: 100013C03PK2022
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Kaur P, Fatmi S, Shakil S, Mandyam S, Abdalslam B. A case of transient right ventricular failure secondary to severe pulmonary hypertension in setting of methamphetamine use. Edorium J Cardiol 2022;7(2):6–10.ABSTRACT
Methamphetamine has been documented to be associated with pulmonary hypertension. Past studies have shown the association of methamphetamine abuse with pulmonary hypertension; however, cases of isolated acute to subacute right heart failure secondary to methamphetamine use have not been documented. Acute to subacute right heart failure, secondary to methamphetamine use itself represents a diagnostic challenge as there is no specific protocol in place for evaluation for pulmonary hypertension secondary to methamphetamine use and high degree of suspicion is needed to differentiate it from other cardio-pulmonary conditions. Echocardiographic findings of increased right ventricular systolic pressure along with morphological findings suggesting cardiac remodeling in the setting of methamphetamine use is highly suspicious of acute to subacute right heart failure. Early recognition and management, along with long-term abstinence from methamphetamine use is critical to prevent chronic effects on myocardium and to prevent further cardiac remodeling. Although dedicated cardiothoracic imaging and cardiac catheterization can be beneficial; neither of these modalities are needed to establish the diagnosis and to initiate primary interventions. Computed tomography (CT) scan however would be beneficial in excluding other causes of pulmonary hypertension, such as primary pulmonary conditions and pulmonary embolism.
Keywords: Dilated right ventricle, Methamphetamine, Paroxysmal nocturnal dyspnea, Pulmonary artery hypertension, Right ventricular failure
INTRODUCTION
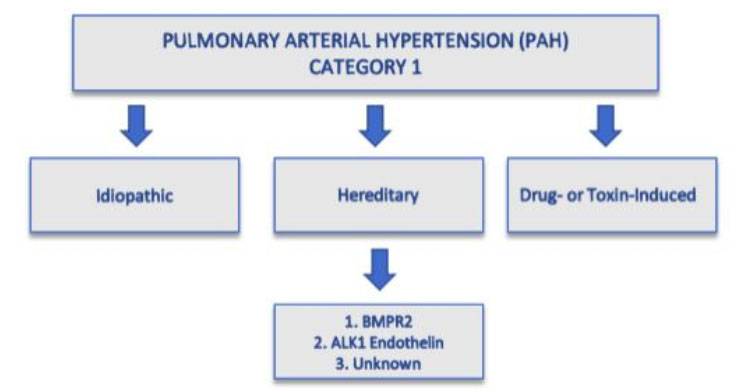
Methamphetamine is a known central nervous system stimulant which is usually prescribed for patients who are diagnosed with neuropsychiatric disorders such as attention deficit hyperactivity syndrome (ADHD) [1]. Methamphetamine is potent and highly addictive in nature and its elicit use is becoming a serious health problem in the United States. In the 2020 National Survey on Drug Use and Health, it was reported that in individuals 12 years or older, about 0.9% (or about 2.6 million individuals) had methamphetamine use disorder in the previous 12 months [2]. The regular use of methamphetamine leads to sympathetic activation of the central nervous system, which may lead to hypertension, cardiac dysrhythmias, myocardial infarction, and ischemic stroke. Methamphetamine is used through various routes including inhalation, smoking, or snorting. One of the most serious documented complications of the drug is pulmonary arterial hypertension (PAH). The World Health Organization (WHO) defines PAH as a resting pulmonary artery pressure greater than 25 mmHg, and it is divided into five categories [3]. Category 1 classification is further subdivided into idiopathic, hereditary, or drug-or toxin-induced causes; however, drug-induced PAH is typically a diagnosis of exclusion [4].
The exact mechanisms of methamphetamine-associated PAH (Meth-APAH) is still unknown. Past studies have shown that methamphetamine uptake is highest within the lungs, possibly contributing to direct pulmonary toxicity and vascular damage [5]. A case of PAH with an association of methamphetamine use was first reported in 1993 [6]. Subsequently, additional retrospective studies have been conducted and they confirmed the association of methamphetamine use and pulmonary hypertension. However, subacute to acute right ventricle failure secondary to severe pulmonary hypertension in the setting of methamphetamine use has not been frequently documented.
CASE REPORT
A 43-year-old male with a past medical history of tobacco presented with progressively worsening shortness of breath and chest pain. The patient complained of substernal chest pain for 3 hours and worsening shortness of breath over the past few days, prior to presentation. He described the chest pain as 10/10 in intensity, non-radiating, and associated with shortness of breath, lightheadedness, and diaphoresis. The patient denied any palpitations, nausea, vomiting, weakness, or dizziness. He also denied any aggravating factors for chest pain, however, stated improvement in his symptoms with rest. In the Emergency Department (ED), he reported using methamphetamine recently multiple times over the past few days and coincided with the initiation of his shortness of breath. He denied associated paroxysmal nocturnal dyspnea (PND), orthopnea, productive cough, diaphoresis, fever, or chills. The patient also denied any significant past medical history and did not have a primary care physician (PCP) and also was unaware of his family history as he was adopted. Although he was noted to have a 30-pack-year smoking history in addition to the methamphetamine use; however, he denied any other illicit drug abuse.
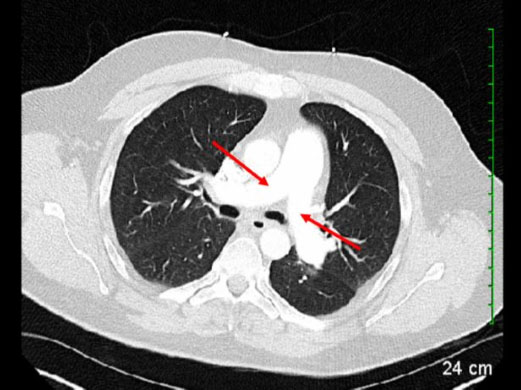
In the ED, laboratory diagnostic data revealed high sensitivity troponin of 95.5 ng/L with serial troponin peaking at 123.5 ng/L [Ref <100 ng/L] and subsequently trending down to within reference range, proBNP was 363, magnesium was 1.8 mg/dL, and white blood count (WBC) was 11.4 u/L. 12-lead electrocardiogram (EKG) revealed sinus tachycardia with right bundle branch block and right axis deviation, although no previous EKGs were available to compare findings. Chest X-ray was negative for any acute cardiopulmonary findings. Computed tomography of the chest was performed to rule out pulmonary embolism and any other underlying pulmonary parenchymal pathology (Figure 1). It showed no underlying pulmonary parenchymal disease, no pulmonary embolism; however, right heart dilation was noted as well dilated pulmonary veins.
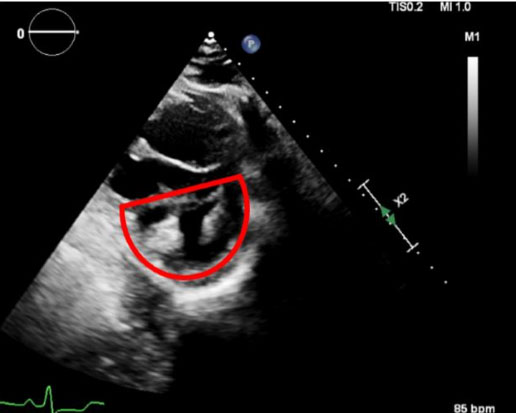
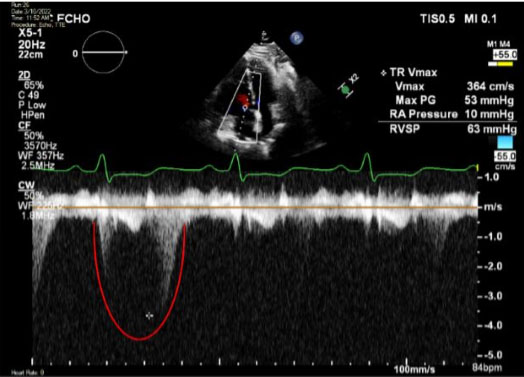
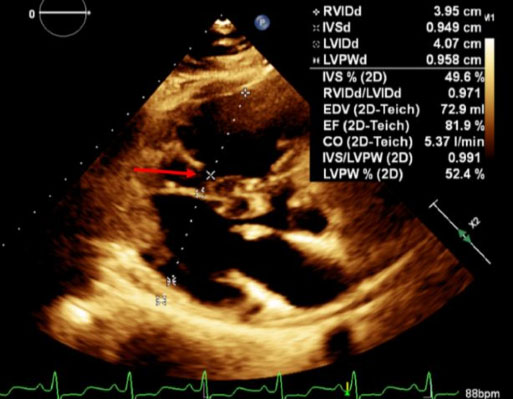
Cardiology was consulted for further evaluation, and the patient underwent a stress test and 2D echocardiography. Stress was negative for any perfusion defects; however, severely dilated right ventricle was noted. Echo also showed a severely dilated right ventricle and it was positive for “D-sign” as shown in Figure 2. In addition, the Echo revealed severe pulmonary hypertension with right ventricle systolic pressure (RVSP) of 63 mmHg and tricuspid regurgitation (TR) jet velocity as shown in Figure 3. Left ventricle ejection fraction was noted to be normal at 60%. 2D Echo also showed a right ventricular diameter of 3.95 cm, as shown in Figure 4.
Per the stress test and Echo findings, no perfusion defects or hypokinesis was noted, along with a prominent right ventricle with severe enlargement; however, with transient troponin elevation, patient was taken for left heart catheterization, which did not reveal any obstructive coronary artery disease. The patient was noted to have severe pulmonary hypertension with no obvious evidence of intracardiac shunt or other cause of pulmonary hypertension. After thorough workup and evaluation by the multidisciplinary team, it was apparent that the patient’s symptoms and right ventricular findings including elevated RVSP and dilation were a complication of methamphetamine use resulting in severe pulmonary hypertension. During the course of hospital stay, the patient was started on antihypertensive medications and his blood pressure was closely monitored for optimal control. He did receive diuresis initially secondary to initial presentation and elevated proBNP; however, the patient was not discharged on diuretics. The patient followed up with cardiology and primary care and had repeat Echo, which showed improvement in RSVP.
DISCUSSION
In this case report, we have described a rare case of methamphetamine associated transient right ventricular failure secondary to pulmonary hypertension. Although methamphetamine use has been known to be associated with myocardial infarction and ischemic changes secondary to its vasoconstrictive properties, this is a rare case of transient isolated right ventricular systolic failure with acute remodeling secondary to methamphetamine-induced severe pulmonary hypertension. Although pulmonary hypertension can be secondary to various etiologies, it is divided into five categories. Drug-induced or toxin-mediated PAH is part of category 1 and typically a diagnosis of exclusion (Figure 5).
Right heart strain can be observed with severe pulmonary hypertension, which can cause right ventricular remodeling and dilation with persistent increase in pulmonary vascular pressures. In the case described, initial clinical workup with CT chest did not demonstrate evidence of large vessel proximal pulmonary embolism, with no evidence of parenchymal changes contributing to pulmonary hypertension were noted. In previous literature, pulmonary hypertension has been documented to be associated with methamphetamine use and based on those findings, there are recommendations now in place, for screening for pulmonary hypertension in patients with history of using methamphetamine [1],[2],[3],[4],[5],[6] [7]. Although association of pulmonary hypertension and methamphetamine has been described, with this case we were able to document findings suggestive of transient acute to subacute right heart systolic failure with all of the associated clinical manifestations. Right ventricular systolic pressure (RVSP) greater than 55–60 mmHg is generally associated with severe pulmonary hypertension and with our patient, RVSP was noted to be 63 mmHg (Figure 2), which is well above the threshold for severe pulmonary hypertension [8],[9],[10]. Similarly, RV dilation as illustrated above in Figure 2 and Figure 4 is also a pathognomonic finding for RV failure that has not been previously described with methamphetamine use. It is also noteworthy that the RV findings we see with our patient represents acute to subacute changes and not chronic changes, as chronic severe pulmonary hypertension would result in RV hypertrophy. Figure 2 also shows the “D-sign” of the septum in the left ventricle resulting from right ventricle overload.
From a clinical perspective, describing a case of acute to subacute right ventricular failure also represents an area where further clinical advancement and innovation can be achieved. Most patients presenting with dyspnea or respiratory symptoms, with the use of methamphetamine can be evaluated with a baseline Echo to assess RV function, RVSP and any possible structural remodeling. This clinical presentation can mimic many other cardio-pulmonary conditions including ischemic presentation. Baseline cardiac workup with EKG and cardiac enzymes in addition to an Echo would be highly beneficial in these cases. Our patient had left heart catheterization after a negative stress test, to completely rule out ischemic etiology. Right heart catheterization in acute to subacute cases would be of minimal benefit, when acute to subacute right ventricular dilation and remodeling from a clear etiology is present; however, there is a role for right heart catheterization in chronic cases and in cases where ischemic pathology is not a concern. To ascertain etiology of pulmonary hypertension, medical management of the above described presentation should be focused toward decreasing RV afterload and addressing pulmonary hypertension acutely, along with cessation of methamphetamine use and proper patient education in the long term. Further research would be beneficial for evaluation of employment of agents that decrease pulmonary vascular resistance that are primarily used in management of primary pulmonary artery hypertension. This can be used as a strategy to acutely address severe pulmonary hypertension and decrease RVSP, which might be beneficial in preventing cardiac remodeling, improving ventricular failure, with better long-term outcomes.
CONCLUSION
The etiology of pulmonary hypertension can be diverse and with this case report, we have described a case of overt systolic right ventricular failure secondary to methamphetamine use. Prompt evaluation of similar presentations in the future will have significant implications in future diagnosis and management. Although most of these cases can be diagnosed with clinical presentation, ruling out ischemic cardiomyopathy is critical and stress test and left heart catheterization can be pivotal. Echocardiogram is also an indispensable tool in the diagnosis of these patients in order to assess RV function. Although previously the gold standard for RV function and pulmonary hypertension assessment was right heart catheterization, most patients do not require right heart catheterization to make the diagnosis in acute to subacute presentations; however, this can be done in chronic cases. This case represents findings associated with methamphetamine use and hence represents a great avenue for intervention and management of patients with isolated right ventricular failure. Right ventricular failure and pulmonary hypertension can eventually lead to congestive heart failure, if not evaluated and managed promptly. As we have described above, there may be a role for agents that are used to treat primary pulmonary hypertension, along with heart failure therapy reducing right ventricular afterload for an acute improvement in symptoms.
REFERENCES
1.
Cheng Y, Tung CK, Chung AKK, et al. Screening of pulmonary hypertension in methamphetamine abusers (SOPHMA): Rationale and design of a multicentre, cross-sectional study. BMJ Open 2019;9(8):e027193. [CrossRef]
[Pubmed]

2.
What is the scope of methamphetamine use in the United States? National Institute on Drug Abuse. 2022. [Available at: https://nida.nih.gov/publications/research-reports/methamphetamine/what-scope-methamphetamine-misuse-in-united-states]

3.
Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 2013;62(25 Suppl):D34–41. [CrossRef]
[Pubmed]

4.
Ryan JJ, Thenappan T, Luo N, et al. The WHO classification of pulmonary hypertension: A case-based imaging compendium. Pulm Circ 2012;2(1):107–21. [CrossRef]
[Pubmed]

5.
Volkow ND, Fowler JS, Wang GJ, et al. Distribution and pharmacokinetics of methamphetamine in the human body: clinical implications. PLoS One 2010;5(12):e15269. [CrossRef]
[Pubmed]

6.
Schaiberger PH, Kennedy TC, Miller FC, Gal J, Petty TL. Pulmonary hypertension associated with long-term inhalation of “crank” methamphetamine. Chest 1993;104(2):614–6. [CrossRef]
[Pubmed]

7.
Ramirez RL 3rd, Perez VDJ, Zamanian RT. Methamphetamine and the risk of pulmonary arterial hypertension. Curr Opin Pulm Med 2018;24(5):416–24. [CrossRef]
[Pubmed]

8.
Huston JH, Maron BA, French J, et al. Association of mild echocardiographic pulmonary hypertension with mortality and right ventricular function. JAMA Cardiol 2019;4(11):1112–21. [CrossRef]
[Pubmed]

9.
Kumar A, Neema PK. Severe pulmonary hypertension and right ventricular failure. Indian J Anaesth 2017;61(9):753–9. [CrossRef]
[Pubmed]

10.
Nathan SD, Shlobin OA, Barnett SD, et al. Right ventricular systolic pressure by echocardiography as a predictor of pulmonary hypertension in idiopathic pulmonary fibrosis. Respir Med 2008;102(9):1305–10. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Paramjit Kaur - Conception of the work, Design of the work, Acquisition of data, Drafting the work, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Syed Fatmi - Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Sidra Shakil - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Saikiran Mandyam - Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Bsmah Abdalslam - Conception of the work, Design of the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestThe authors declare that the case study was not associated with any commercial or financial relationships that could be construed as potential conflict of interest.
Copyright© 2022 Paramjit Kaur et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.